COVID-19 - Latest - Google News
December 01, 2021 at 11:21AM
https://ift.tt/3rm7cuI
COVID-19 Testing May Be Required for Travelers Entering U.S. - NBC New York
COVID-19 - Latest - Google News
https://ift.tt/2VQ2gy8
Copyright © 2021 NBCUniversal Media, LLC. All rights reserved
/cloudfront-us-east-1.images.arcpublishing.com/gray/QQ6QA72CTBCVZPNDQN3V322IBA.jpg)
RAPID CITY, S.D. (KEVN) - As the Delta variant continues to dominate South Dakota’s COVID cases, a new one has appeared.
The Omicron variant was recently discovered in South Africa and has quickly spread to nearby countries, and is now reported in Canada.
As these variant infections grow, officials have little information about them.
“It’s different from the Delta, it has 30 changes to the spike protein compared to only 10 for the Delta and that’s the concern. Some of them are similar to the Delta, what we do not know is it more transmissible and is it going to cause more severe disease,” said Dr. Shankar Kurra, vice president of medical affairs at Monument Health.
New variants of the COVID-19 virus aren’t a surprise, as people travel through open borders, it is nearly impossible to keep “the genie in the bottle”.
But, is the Delta variant, which is easier to spread and causes worse symptoms, the milder strain compared to the new Omicron variant?
“Those are all unanswered questions and really until we know more about it, it’s hard to say what this will really bring to people in our state,” said Kim Malsam-Rysdon, secretary of health for South Dakota Department of Health.
Viruses constantly change, creating new variants. Some disappear and some stick around.
Kurra and Malsam-Rysdon say the Omicron variant is probably in the country already, but not reported.
When it eventually comes to South Dakota, the Department of Health plans to continue the precautions stressed at the beginning of the pandemic.
“Certainly there are other things that people could be doing, we can be washing our hands often, staying home if you’re sick, wearing a mask if you can’t stay away from other folks, so those things are all still important,” said Malsam-Rysdon.
And both health officials say the best plan of action is to get vaccinated.
“What the vaccine does is, one, it prevents transmission, number two, it prevents hospitalization, the biggest risk we stand if Omicron were to overtake the Delta variant, that we’ll have more hospitalizations,” said Kurra.
And while people are getting their COVID shot, Malsam-Rysdon advises everyone to get the flu shot too.
Copyright 2021 KEVN. All rights reserved.
/cloudfront-us-east-2.images.arcpublishing.com/reuters/GW2ZDWZYSBLIXNV7DCYAQI6BDY.jpg)
Nov 30 (Reuters) - The Biden administration was blocked on Tuesday from enforcing two mandates requiring millions of American workers to get vaccinated against COVID-19, a key part of its strategy for controlling the spread of the coronavirus.
U.S. District Judge Terry Doughty in Monroe, Louisiana, temporarily blocked the Centers for Medicare & Medicaid Services (CMS) from enforcing its vaccine mandate for healthcare workers until the court can resolve legal challenges.
Doughty's ruling applied nationwide, except in 10 states where the CMS was already prevented from enforcing the rule due to a prior order from a federal judge in St. Louis.
Doughty said the CMS lacked the authority to issue a vaccine mandate that would require more than 2 million unvaccinated healthcare workers to get a coronavirus shot.
"There is no question that mandating a vaccine to 10.3 million healthcare workers is something that should be done by Congress, not a government agency," wrote Doughty.
Separately, U.S. District Judge Gregory Van Tatenhove in Frankfort, Kentucky, blocked the administration from enforcing a regulation that new government contracts must include clauses requiring that contractors' employees get vaccinated.
The contractor ruling applied in the three states that had filed the lawsuit, Kentucky, Ohio and Tennessee, one of at least 13 legal challenges nationwide against the regulation. It appears to be the first ruling against the contractor vaccine mandate.
The White House declined to comment.
The legal setbacks for President Joe Biden's vaccine policy come as concerns that the Omicron coronavirus variant could trigger a new wave of infections and curtail travel and economic activity across the globe.
Biden unveiled regulations in September to increase the U.S. adult vaccination rate beyond the current 71% as a way of fighting the pandemic, which has killed more than 750,000 Americans and weighed on the economy.
Republican state attorneys general, conservative groups and trade organizations have sued to stop the regulations.
Tuesday's rulings add to a string of court losses for the Biden administration over its COVID-19 policies.
The most sweeping regulation, a workplace vaccine-or-testing mandate for businesses with at least 100 employees, was temporarily blocked by a federal appeals court in early November.
In August, the U.S. Supreme Court ended the administration's pandemic-related federal moratorium on residential evictions.
Reporting by Tom Hals in Wilmington, Delaware; Additional reporting by Nandita Bose in Washington; Editing by Jonathan Oatis and Peter Cooney

Mayor-elect Eric Adams is thousands of miles away traveling in the Republic of Ghana, but even as he embarks on a trip he says will help him connect to his ancestral roots, Adams is inching closer to finalizing top picks in his administration.
Sources tell NY1 Adams is seriously considering Lorraine Grillo as an option for first deputy mayor. She's an experienced and respected government operative with long standing ties to the city's massive web of bureaucracy. Grillo formerly led the Schools Construction Authority and was recently appointed as the city's COVID recovery czar.
Grillo would bring decades of experience to a position tasked with ensuring the delivery of essential services across city agencies and managing the city's workforce.
Also in the running is Julie Samuels, executive director of TECHNYC, a nonprofit which works to grow the technology sector and attract tech talent to the city. Sources say Samuels could be tapped to serve as Deputy Mayor for Technology.
Ester Fuchs, director of the Urban and Social Policy Program at Columbia University’s School of International and Public Affairs, who served as special advisor to Mayor Bloomberg, said the work to set up a new government goes far beyond naming commissioners and deputy mayors.
"Adams has to deal with the immediate service delivery challenges," Fuchs said. "He's got to set up City Hall in a managerial structure that he's comfortable with, not everybody can report to the mayor."
As he travels the West African nation, aides to Adams said he's hard at work continuing his search for candidates and finalizing top picks.
"You're doing a lot of new hiring at the highest levels of city government. You're looking for the head of EDC and your commissioners," Fuchs said.
Adams left the city Monday night for what he said is a spiritual journey of sorts for an incoming mayor known for daily mediation.
"This is a spiritual journey for me," Adams said Monday. "My ancestors came here in the bottom of slave ships and 400 years later I am the mayor of one of the most important cities in New York. I am going there to pray, I am going there to do some spiritual cleansing."
Those who know what it takes to set up the city's massive government structure say the time for a break is now.
"I'm not that worried about this trip," Fuchs said. "To be fair, if this is a spiritual thing for him and it's to strengthen him and gets him ready for round one of what is going to be a very difficult transition I'm all for it, so get your energy."
As mayor, Adams will be in charge of more than 50 city agencies, dozens of offices and hundreds of appointments.
Stephen Scherr, chief financial officer of Goldman Sachs, is being considered for housing and economic development. He already sits on Adams' transition team. Also under consideration is Frank Carone, Adams' personal lawyer and right hand man. He could be tapped as the incoming mayor's chief of staff.
Adams will be in Ghana all week and return on the 8th. It's not yet clear if he will hold any official functions with Ghanaian officials.

Covid-19 positivity rates have been increasing in the city and state in recent months, but the city’s health systems said cases have been within their capabilities to handle. They added that even if the omicron variant adds a surge on top of Delta, they do not anticipate any disruptions in supplies or services downstate.
As of Sunday, the state’s seven-day Covid-19 test positivity rate average exceeded 4%—a level last seen around May.
“This upswing hasn’t been surprising,” said Dr. Bruce Lee, professor of health policy and management at the CUNY Graduate School of Public Health. Evidence suggests respiratory viruses increase in transmission during drier and colder weather, Lee said, and people staying indoors more as Covid precautions relaxed probably drove rates up.
“Public health planners had already anticipated a winter surge,” he said.
But local health systems cited adequate capacity to handle the recent increase in cases, especially downstate. The city’s seven-day positivity rate was about 2%, according to state data.
“We’re not even close to filling up our capacity that we saw in spring last year,” said Dr. Bruce Farber, chief of infectious diseases at Northwell Health. As of Monday, the Long Island health system was on average at 82% capacity. The majority of recent Covid cases have been unvaccinated individuals, but there was no need to curtail any services, Farber said.
A big part of the ease had to do with experience, said Dr. Laura Iavicoli, assistant vice president of emergency management at NYC Health + Hospitals.
“This looks like the beginning of a fourth wave,” Iavicoli said, “and given our modeling, it looks like we will not surpass two-thirds of what we saw in the third wave this summer.”
Gov. Kathy Hochul’s declaration of a state of emergency, permitting hospitals to implement a flex and surge strategy and cancel elective procedures if needed, was probably less relevant to downstate hospitals, said Dr. Brian Bosworth, chief medical officer at NYU Langone Health.
“The governor said she wanted the flex to help hospitals that were in danger of running out of beds adjust capacity,” Bosworth said. “That seemed to concern mostly institutions upstate.”
Local health systems also said they had adequate supplies and personal protective equipment for the current surge and beyond.
Dr. Bernard Camins, medical director of infection prevention at Mount Sinai Health System, said the institution had a stable supply since the summer of last year, having drawn lessons from the shortage experienced during the spring surge of 2020.
What local institutions are keeping an eye out for, however, is how the omicron variant plays out in the city.
“It’s too early to say omicron will cause a surge,” Lee said. Although early reports suggest it might have increased transmissibility compared with Delta, it is not clear it can outcompete the other variants circulating, he said.
“People were worried the episilon variant seen in California was going to spread nationwide, but that got outcompeted by Delta instead,” he noted.
“One thing is clear is that the recent upswing is over 99% Delta,” Iavicoli said. That variant spread is still not over, she said, adding New Yorkers need to remain vigilant about masking as they head into the winter.
In case omicron does result in another surge, health systems are beginning preparations. NYU Langone is considering increasing the amount of variant sequencing it does with its positive tests, Bosworth said. Mount Sinai’s pathogen surveillance team is in the process of expanding its surveillance lab capacity to detect the omicron variant earlier, Camins said.
Bed capacity remains top of mind, and system-wide briefings on how to turn beds in units for Covid use have been distributed, Iavicoli said. Similarly, Northwell has playbooks available to extend its bed count to levels seen during the spring surge last year, to more than 5,000 beds, a Northwell spokeswoman said.
It’s never too early to start preparing for the omicron variant, Bosworth said, adding it could already be on our shores.
[unable to retrieve full-text content]
South Korea’s daily virus jump exceeds 5,000 for first time The Seattle Times[unable to retrieve full-text content]
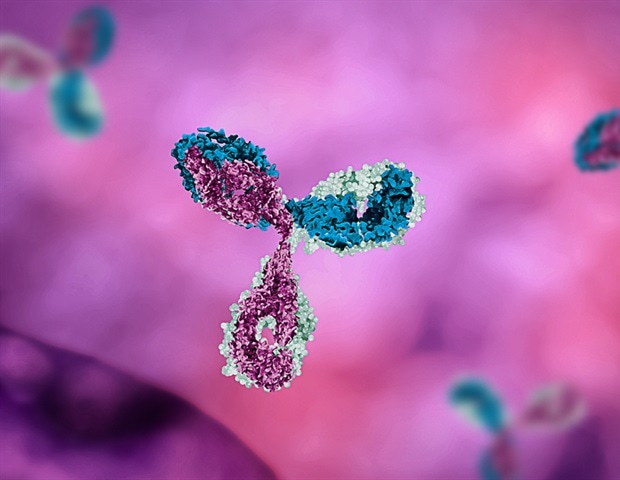
It is widely understood that antibodies neutralize viruses by latching onto their surfaces and blocking them from infecting host cells. But new research reveals that this barrier method isn't the only way that antibodies disable viruses. An international team of researchers led by Penn State has discovered that antibodies also distort viruses, thereby preventing them from properly attaching to and entering cells.
Everybody thinks of antibodies as binding to viruses and blocking them from entering cells -; essentially locking them down. But our research reveals for the first time that antibodies may also physically distort viruses, so they are unable to properly attach to and infect host cells."
Ganesh Anand, associate professor of chemistry, Penn State
In their study, which published online today (Nov. 30) in the journal Cell, Anand and his colleagues investigated the interactions between human monoclonal antibody (HMAb) C10 and two disease-causing viruses: Zika and dengue. The HMAb C10 antibodies they used had previously been isolated from patients infected with dengue virus and had also been shown to neutralize Zika virus.
The researchers used a combination of techniques, including cryogenic electron microscopy (cryo-EM) to visualize the viruses and hydrogen/deuterium exchange mass spectrometry (HDXMS) to understand their movement.
"Cryo-EM involves flash-freezing a solution containing molecules of interest and then targeting them with electrons to generate numerous images of individual molecules in different orientations," explained Anand. "These images are then integrated into one snapshot of what the molecule looks like. The technique provides much more accurate pictures of molecules than other forms of microscopy."
To document the effects of antibodies on Zika and dengue viruses, the team collected cryo-EM snapshots of the viruses under conditions of increasing concentrations of antibodies.
In parallel, the team applied HDXMS, a technique in which molecules of interest -; in this case Zika and dengue virus, along with HMAb C10 antibodies -; are submerged in heavy water. Heavy water, Anand explained, has had its hydrogen atoms replaced with deuterium, hydrogen's heavier isotopic cousin.
"When you submerge a virus in heavy water, the hydrogen atoms on the surface of the virus exchange with deuterium," he said. "You can then use mass spectrometry to measure the heaviness of the virus as a function of this deuterium exchange. By doing this, we observed that dengue virus, but not Zika virus, became heavier with deuterium as more antibodies were added to the solution. This suggests that for dengue virus, the antibodies are distorting the virus and allowing more deuterium to get in. It's as if the virus is getting squished and more surface area becomes exposed where hydrogen can be exchanged for deuterium."
In contrast, Zika virus did not become heavier when placed in heavy water, suggesting that its surface, while fully occupied by antibodies, is not distorted by the antibodies.
Anand explained that by combining cryo-EM and HDXMS, the team was able to get a comprehensive picture of what happens when antibodies attach to Zika and dengue viruses.
"It's like those cartoon flipbooks, where each page has a slightly different image, and when you flip through the book, you see a short movie," he said. "Imagine a flipbook with drawings of a racehorse. Cryo-EM shows you what the racehorse looks like and HDXMS shows you how fast the racehorse is moving. You need both techniques to be able to describe a racehorse in motion. This complementary set of tools enabled us to understand how one type of antibody differentially affects two types of viruses."
He noted that the fact that the more antibodies they added, the more distorted the dengue virus particles became, suggests that stoichiometry -; the relationship between the quantities of the reactants and the products before, during and after a chemical reaction -; matters.
"It's not enough to just have antibodies present," he said. "How much antibody you add determines the extent of neutralization."
In fact, the team found that at saturating conditions, in which antibodies were added at high enough concentrations to fill all the available binding locations on the dengue viruses, 60% of the virus' surfaces became distorted. This distortion was enough to protect the cells from infection.
"If you have enough antibodies, they will distort the virus particle enough so that it's preemptively destabilized before it even reaches its target cells," Anand said.
Indeed, when the scientists incubated the antibody-bound dengue viruses with BHK-21 cells, a cell line from the kidneys of baby hamsters that is often used in viral infection research, they found that 50-70% fewer cells were infected.
Anand explained that with some viruses, including Zika, antibodies work by jamming the exits so the passenger cannot get out of the car. We have found a new mechanism in dengue virus whereby antibodies basically total the car so it cannot even travel to a cell."
How are the antibodies distorting the dengue virus particles?
Anand explained that contrary to the now-familiar SARS-CoV-2, which has spike proteins protruding in all directions, the surfaces of both Zika and dengue is a smoother surface with peaks and valleys.
Anand noted that for dengue virus, antibodies especially prefer binding the 'peaks' known as 5-fold vertices. Once all the proteins on the 5-fold vertices have been bound, antibodies will turn to their second-favorite peaks -; the 3-fold vertices. Finally, they are left with only the 2-fold vertices.
"Antibodies do not like two-fold vertices because they are very mobile and difficult to bind to," said Anand. "We found that once the 5- and 3-fold vertices have been fully bound with antibodies, if we add more antibodies to the solution, the virus starts to shudder. There's this competition taking place between antibodies trying to get in and the virus trying to shake them off. As a result, these antibodies end up burrowing into the virus rather than binding onto the 2-fold vertices, and we think it's this digging into the virus particle that causes the virus to shake and distort and ultimately become non-functional."
What is the difference between Zika and dengue?
Anand explained that Zika is a much more stable, less dynamic virus than dengue, which has a lot of moving parts.
"Dengue and Zika look similar but each one has a different give. Dengue may have evolved as a more mobile virus as a way of avoiding being caught by antibodies. Its moving parts confuse and throw off the immune system. Unfortunately for dengue, antibodies have evolved a way around this by burrowing into the virus and distorting it."
It appears, he said, that the same type of antibody can neutralize Zika and dengue in two different ways -; one where it binds to the virus and deactivates it, which is the traditional way we think about antibody activity, and the other where it burrows in and distorts the virus.
What about other viruses?
Anand said the distortion strategy his team discovered may be used by antibodies when they are confronted with other types of viruses as well.
"Dengue is just a model virus that we used in our experiments, but we think this preemptive destabilization strategy may be broadly applicable to any virus," he said. "It may be that the antibodies first attempt to neutralize viruses through the barrier method and if they are unsuccessful, they resort to the distortion method."
Are there any potential applications of the findings?
The findings could be useful in designing therapeutic antibodies, Anand said.
"HMAb C10 antibodies are specific to dengue and Zika viruses, and happen to be capable of neutralizing Zika and dengue viruses in two different ways," he said. "But you could potentially design therapeutics with the same capabilities for treating other diseases, such as COVID-19. By creating a therapeutic with antibodies that can both block and distort viruses, we can possibly achieve greater neutralization."
He added, "You don't want to wait for a virus to reach its target tissue, so if you can introduce such a therapeutic cocktail as a nasal spray where the virus first enters the body, you can prevent it from even entering the system. By doing this, you may even be able to use less antibody since our research shows that it takes less antibody to neutralize a virus through the distortion method. You can get better bang for the buck."
Overall, Anand stressed that the importance of the study is that it reveals an entirely new strategy that some antibodies use to disable some viruses.
"Previously, all we knew about antibodies was that they bind and neutralize viruses," he said. "Now we know that antibodies can neutralize viruses in at least two different ways, and perhaps even more. This research opens the door to a whole new avenue of exploration."

By CARLA K. JOHNSON
After a slow start, the United States has improved its surveillance system for tracking new coronavirus variants such as omicron, boosting its capacity by tens of thousands of samples per week since early this year.
Viruses mutate constantly. To find and track new versions of the coronavirus, scientists analyze the genetic makeup of a portion of samples that test positive.
They’re looking at the chemical letters of the virus’s genetic code to find new worrisome mutants, such as omicron, and to follow the spread of known variants, such as delta.
It’s a global effort, but until recently the U.S. was contributing very little. With uncoordinated and scattershot testing, the U.S. was sequencing fewer than 1% of positive specimens earlier this year. Now, it is running those tests on 5% to 10% of samples. That’s more in line with what other nations have sequenced and shared with global disease trackers over the course of the pandemic.
“Genomic surveillance is strong,” said Kelly Wroblewski, director of infectious diseases at the Association of Public Health Laboratories.
Contributing to the effort are nearly 70 state and local public health labs, which are sequencing 15,000 to 20,000 specimens each week. Other labs, including those run by the Centers for Disease Control and Prevention and its contractors, bring the total to 40,000 to 80,000 weekly.
Nine months ago, about 12,000 samples each week were being analyzed in this way.
“We’re in a much, much better place than a year ago or even six or nine months ago,” said Kenny Beckman of the University of Minnesota, who credited federal dollars distributed to public and private labs. He directs the university’s genomics laboratory, which now sequences about 1,000 samples a week from states including Minnesota, Arkansas and South Dakota. A year ago, the lab did no sequencing.
Relying on $1.7 billion in President Joe Biden’s coronavirus relief bill, the U.S. has been setting up a national network to better track coronavirus mutations.
Still, about two dozen countries are sequencing a larger proportion of positive samples than the U.S., said Dr. William Moss of the Johns Hopkins Bloomberg School of Public Health. Omicron’s emergence could “stimulate the United States to do this better.”
“I think we still have a long way to go,” Moss said.
Some states are sequencing only about 1% of samples while others are in the range of 20%, noted Dr. Phil Febbo, chief medical officer for Illumina, a San Diego-based company that develops genomic sequencing technologies.
“We could be more systematic about it and more consistent so we ensure there are no genomic surveillance deserts where we could miss the emergence of a variant,” Febbo said.
Aiding the surveillance effort, standard PCR tests that use nasal swabs sent to laboratories can detect a sign that someone probably has the omicron variant. If a PCR test is positive for only two of the three target genes — a so-called S-dropout test result — it’s a marker for omicron even before the extra step of genetic sequencing to prove it.
“It’s fortuitous,” said Trevor Bedford, a biologist and genetics expert at Fred Hutchinson Cancer Research Center. “If you need to do sequencing to identify the variant you’re always going to be lagged a bit and it’s going to be more expensive. If you just rely on this S-dropout as identification then it’s easier.”
He said other variants also have sparked this quirk in PCR test results, but not the delta variant. With delta so dominant in the U.S. right now, an S-dropout result will get noticed, Bedford said. (Bedford receives funding from the Howard Hughes Medical Institute, which also supports The Associated Press Health and Science Department.)
Dr. Anthony Fauci, the nation’s top infectious disease expert, said it is “inevitable” that omicron will make its way into the United States.
Many experts said it’s probably already here and will be picked up by the surveillance system soon. But the question is, then what?
University of Wisconsin AIDS researcher David O’Connor noted: “We don’t have the sorts of interstate travel restrictions that would make it possible to contain the virus in any one place.”
Instead, genomic surveillance will tell officials if omicron is spreading unusually fast somewhere and whether more resources should be sent to those places, he said.
When omicron does surface, public health authorities will have to consider other variables in their triage efforts, such as the level of infection already present in that community and the vaccination rate. Serious outbreaks in highly vaccinated areas would be particularly concerning.
Still, the University of Minnesota’s Beckman sees little upside in vastly ramping up sequencing.
“You don’t need to sequence more than a few percent of positive cases to get a feel for how quickly it’s growing,” he said.
Unlike in some other countries, U.S. government officials haven’t exercised the authority to force people to quarantine if they test positive for worrisome variants. Given that, sequencing is mainly a surveillance tool for tracking mutations’ spread.
“I think it’s important to track variants, but I don’t think it’s practical to think that we’re going to be able to sequence quickly and broadly enough to stop a variant in its tracks,” Beckman said.
___
AP writers Lauran Neergaard, Matthew Perrone and Ricardo Alonso-Zaldivar contributed.
___
The Associated Press Health and Science Department receives support from the Howard Hughes Medical Institute’s Department of Science Education. The AP is solely responsible for all content.
A new variant named omicron (B.1.1.529) was reported by researchers in South Africa on Nov. 24, 2021, and designated a “variant of concern” by the World Health Organization two days later. Omicron is very unusual in that it is by far the most heavily mutated variant yet of SARS-CoV-2, the virus that causes COVID-19.
The omicron variant has 50 mutations overall, with 32 mutations on the spike protein alone. The spike protein – which forms protruding knobs on the outside of the SARS-CoV-2 virus – helps the virus adhere to cells so that it can gain entry. It is also the protein that all three vaccines currently available in the U.S. use to induce protective antibodies. For comparison, the delta variant has nine mutations. The larger number of mutations in the omicron variant may mean that it could be more transmissible and/or better at evading immune protection – a prospect that is very concerning.
I am a virologist who studies emerging and zoonotic viruses to better understand how new epidemic or pandemic viruses emerge. My research group has been studying various aspects of the COVID-19 virus, including its spillover into animals.
While the unusually high number of mutations in the omicron variant is surprising, the emergence of yet another SARS-CoV-2 variant is not unexpected.
Through natural selection, random mutations accumulate in any virus. This process is sped up in RNA viruses, including SARS-CoV-2. If and when a set of mutations provides a survival advantage to a variant over its predecessors, the variant will out-compete all other existing virus variants.
Does the omicron variant’s greater number of mutations mean it is more dangerous and transmissible than delta? We simply don’t know yet. The conditions that led to the emergence of the variant are not yet clear, but what is clear is that the shear number and configuration of mutations in omicron is unusual.
One possible explanation for how viral variants with multiple mutations emerge is through prolonged infection in a patient whose immune system is suppressed – a situation that can lead to rapid viral evolution. Researchers have hypothesized that some of the earlier SARS-CoV-2 variants, such as the alpha variant, may have stemmed from a persistently infected patient. However, the unusual constellation and numerous mutations in the omicron variant make it very different from all other SARS-CoV-2 strains, which raises questions about how it came about.
Another possible source of variants could be through animal hosts. The virus that causes COVID-19 can infect several animal species, including mink, tigers, lions, cats and dogs. In a study that is not yet peer-reviewed, an international team that I lead recently reported widespread infection by SARS-CoV-2 in free-living and captive white-tailed deer in the U.S. Therefore, we also cannot rule out the possibility that the omicron variant emerged in an animal host through rapid evolution.
Delta is between 40% and 60% more transmissible than the alpha variant and nearly twice as transmissible as the original SARS-CoV-2 virus first identified in China. The delta variant’s heightened transmissibility is the primary reason why researchers believe it was able to out-compete other variants to become the dominant strain.
A key factor in viral fitness is its replication rate – or how quickly a virus can make more copies of itself. The delta variant replicates faster than previous SARS-CoV-2 variants, and a not-yet-peer-reviewed study estimated that it produces 1,000 times more virus particles than its predecessors.
In addition, people infected with the delta variant are making and shedding more virus, which is another potential mechanism for its increased ability to spread. Research suggests that a possible explanation for the delta variant’s heightened ability to replicate is that mutations in the spike protein led to more efficient binding of the spike protein to its host, via the ACE-2 receptor.
The delta variant has also acquired mutations that would allow it to evade neutralizing antibodies that serve a critical role in the body’s defense against an invading virus. This could explain why, as multiple reports have shown, the COVID-19 vaccines have been somewhat less effective against the delta variant. This combination of high transmissibility and immune evasion could help explain how the delta variant became so successful.
Studies also show that people infected with the delta variant have a higher risk of being hospitalized compared to those infected with the original SARS-CoV-2 and early variants. One particular mutation on the spike protein of the delta variant – the P681R mutation – is thought to be a key contributor to its improved ability to enter cells and to cause more severe disease.
It is too early to say if the omicron variant is fitter than delta or if it will become dominant. Omicron shares some mutations with the delta variant but also possesses others that are quite different. But one of the reasons why we in the research community are particularly concerned is that the omicron variant has 10 mutations in the receptor-binding domain – the part of the spike protein that interacts with the ACE-2 receptor and mediates entry into cells – compared with just two for the delta variant.
[Too busy to read another daily email? Get one of The Conversation’s curated weekly newsletters.]
Suppose the combination of all the mutations in omicron makes it either more transmissible or better at immune evasion than delta. In that case, we could see the spread of this variant globally. However, it is also possible that the unusually high number of mutations could be detrimental to the virus and make it unstable.
It is highly likely that the omicron variant is not the endgame and that more SARS-CoV-2 variants will emerge. As SARS-CoV-2 continues to spread among humans, natural selection and adaptation will result in more variants that could plausibly be more transmissible than delta.
We know from influenza viruses that the process of viral adaptation never ends. Lower vaccination rates among many countries means that there are still a lot of susceptible hosts out there for the virus, and that it will continue to circulate and mutate as long as it can spread. The emergence of the omicron variant is yet another reminder of the urgency to vaccinate to stop the further spread and evolution of SARS-CoV-2.
In-school vaccination clinics were so popular during the first round earlier this month that the city decided to bring them back to hundreds of schools, including PS 40 in Gramercy.
Right now, only 16% percent of NYC school kids age 5 to 11 have gotten their first shot, and officials want to dramatically boost those numbers.
ALSO READ | No confirmed cases of omicron variant in NYC, but new mask advisory issued
School vaccine schedules can be found at Schools.nyc.gov/COVID19, and school leaders are also sending home communications with students.
Meantime, four months after the city staged a massive reopening concert, Mayor Bill de Blasio is asking people to put their masks back on.
The mayor says 88% of New York City adults have gotten at least one shot, and close to a million have received boosters. Still, the number of new cases in unvaccinated people far exceeds instances among fully vaccinated people.
So far, New York has no confirmed cases of the omicron variant, but experts say it's only a matter of time, with initial data suggesting this variant may spread even easier than the delta variant.
Health experts say your best defense remains vaccination and boosters.
"We don't know exactly what's going on with this variant, but I would assume -- and I think it's a reasonable assumption -- that when you get vaccinated and boosted and your level goes way up, you're going to have some degree of protection, at least against severe disease," Dr. Anthony Fauci said.
ALSO READ | 2 men impersonating NYPD officers rob home in the Bronx: New video
"Preliminary evidence suggests that those who've had COVID-19 in the past may be more easily re-infected with omicron," he said.

Centers for Disease Control and Prevention on coronavirus
Submit a News Tip or Question
Copyright © 2021 WABC-TV. All Rights Reserved.

Covid-19 positivity rates have been increasing in the city and state in recent months, but the city’s health systems said cases have been within their capabilities to handle. They added that even if the omicron variant adds a surge on top of Delta, they do not anticipate any disruptions in supplies or services downstate.
As of Sunday, the state’s seven-day Covid-19 test positivity rate average exceeded 4%—a level last seen around May.
“This upswing hasn’t been surprising,” said Dr. Bruce Lee, professor of health policy and management at the CUNY Graduate School of Public Health. Evidence suggests respiratory viruses increase in transmission during drier and colder weather, Lee said, and people staying indoors more as Covid precautions relaxed probably drove rates up.
“Public health planners had already anticipated a winter surge,” he said.
But local health systems cited adequate capacity to handle the recent increase in cases, especially downstate. The city’s seven-day positivity rate was about 2%, according to state data.
“We’re not even close to filling up our capacity that we saw in spring last year,” said Dr. Bruce Farber, chief of infectious diseases at Northwell Health. As of Monday, the Long Island health system was on average at 82% capacity. The majority of recent Covid cases have been unvaccinated individuals, but there was no need to curtail any services, Farber said.
A big part of the ease had to do with experience, said Dr. Laura Iavicoli, assistant vice president of emergency management at NYC Health + Hospitals.
“This looks like the beginning of a fourth wave,” Iavicoli said, “and given our modeling, it looks like we will not surpass two-thirds of what we saw in the third wave this summer.”
Gov. Kathy Hochul’s declaration of a state of emergency, permitting hospitals to implement a flex and surge strategy and cancel elective procedures if needed, was probably less relevant to downstate hospitals, said Dr. Brian Bosworth, chief medical officer at NYU Langone Health.
“The governor said she wanted the flex to help hospitals that were in danger of running out of beds adjust capacity,” Bosworth said. “That seemed to concern mostly institutions upstate.”
Local health systems also said they had adequate supplies and personal protective equipment for the current surge and beyond.
Dr. Bernard Camins, medical director of infection prevention at Mount Sinai Health System, said the institution had a stable supply since the summer of last year, having drawn lessons from the shortage experienced during the spring surge of 2020.
What local institutions are keeping an eye out for, however, is how the omicron variant plays out in the city.
“It’s too early to say omicron will cause a surge,” Lee said. Although early reports suggest it might have increased transmissibility compared with Delta, it is not clear it can outcompete the other variants circulating, he said.
“People were worried the episilon variant seen in California was going to spread nationwide, but that got outcompeted by Delta instead,” he noted.
“One thing is clear is that the recent upswing is over 99% Delta,” Iavicoli said. That variant spread is still not over, she said, adding New Yorkers need to remain vigilant about masking as they head into the winter.
In case omicron does result in another surge, health systems are beginning preparations. NYU Langone is considering increasing the amount of variant sequencing it does with its positive tests, Bosworth said. Mount Sinai’s pathogen surveillance team is in the process of expanding its surveillance lab capacity to detect the omicron variant earlier, Camins said.
Bed capacity remains top of mind, and system-wide briefings on how to turn beds in units for Covid use have been distributed, Iavicoli said. Similarly, Northwell has playbooks available to extend its bed count to levels seen during the spring surge last year, to more than 5,000 beds, a Northwell spokeswoman said.
It’s never too early to start preparing for the omicron variant, Bosworth said, adding it could already be on our shores.
In-school vaccination clinics were so popular during the first round earlier this month that the city decided to bring them back to hundreds of schools, including PS 40 in Gramercy.
Right now, only 16% percent of NYC school kids age 5 to 11 have gotten their first shot, and officials want to dramatically boost those numbers.
ALSO READ | No confirmed cases of omicron variant in NYC, but new mask advisory issued
School vaccine schedules can be found at Schools.nyc.gov/COVID19, and school leaders are also sending home communications with students.
Meantime, four months after the city staged a massive reopening concert, Mayor Bill de Blasio is asking people to put their masks back on.
The mayor says 88% of New York City adults have gotten at least one shot, and close to a million have received boosters. Still, the number of new cases in unvaccinated people far exceeds instances among fully vaccinated people.
So far, New York has no confirmed cases of the omicron variant, but experts say it's only a matter of time, with initial data suggesting this variant may spread even easier than the delta variant.
Health experts say your best defense remains vaccination and boosters.
"We don't know exactly what's going on with this variant, but I would assume -- and I think it's a reasonable assumption -- that when you get vaccinated and boosted and your level goes way up, you're going to have some degree of protection, at least against severe disease," Dr. Anthony Fauci said.
ALSO READ | 2 men impersonating NYPD officers rob home in the Bronx: New video
"Preliminary evidence suggests that those who've had COVID-19 in the past may be more easily re-infected with omicron," he said.

Centers for Disease Control and Prevention on coronavirus
Submit a News Tip or Question
Copyright © 2021 WABC-TV. All Rights Reserved.
/cloudfront-us-east-1.images.arcpublishing.com/gray/SYZGZ6MXMFFQZFDYDE3QEIDSHE.jpg)
(AP) – After a slow start, the United States has improved its surveillance system for tracking new coronavirus variants such as omicron, boosting its capacity by tens of thousands of samples per week since early this year.
Viruses mutate constantly. To find and track new versions of the coronavirus, scientists analyze the genetic makeup of a portion of samples that test positive.
They’re looking at the chemical letters of the virus’s genetic code to find new worrisome mutants, such as omicron, and to follow the spread of known variants, such as delta.
It’s a global effort, but until recently the U.S. was contributing very little. With uncoordinated and scattershot testing, the U.S. was sequencing fewer than 1% of positive specimens earlier this year. Now, it is running those tests on 5% to 10% of samples. That’s more in line with what other nations have sequenced and shared with global disease trackers over the course of the pandemic.
“Genomic surveillance is strong,” said Kelly Wroblewski, director of infectious diseases at the Association of Public Health Laboratories.
Contributing to the effort are nearly 70 state and local public health labs, which are sequencing 15,000 to 20,000 specimens each week. Other labs, including those run by the Centers for Disease Control and Prevention and its contractors, bring the total to 40,000 to 80,000 weekly.
Nine months ago, about 12,000 samples each week were being analyzed in this way.
“We’re in a much, much better place than a year ago or even six or nine months ago,” said Kenny Beckman of the University of Minnesota, who credited federal dollars distributed to public and private labs. He directs the university’s genomics laboratory, which now sequences about 1,000 samples a week from states including Minnesota, Arkansas and South Dakota. A year ago, the lab did no sequencing.
Relying on $1.7 billion in President Joe Biden’s coronavirus relief bill, the U.S. has been setting up a national network to better track coronavirus mutations.
Still, about two dozen countries are sequencing a larger proportion of positive samples than the U.S., said Dr. William Moss of the Johns Hopkins Bloomberg School of Public Health. Omicron’s emergence could “stimulate the United States to do this better.”
“I think we still have a long way to go,” Moss said.
Some states are sequencing only about 1% of samples while others are in the range of 20%, noted Dr. Phil Febbo, chief medical officer for Illumina, a San Diego-based company that develops genomic sequencing technologies.
“We could be more systematic about it and more consistent so we ensure there are no genomic surveillance deserts where we could miss the emergence of a variant,” Febbo said.
Aiding the surveillance effort, standard PCR tests that use nasal swabs sent to laboratories can detect a sign that someone probably has the omicron variant. If a PCR test is positive for only two of the three target genes — a so-called S-dropout test result — it’s a marker for omicron even before the extra step of genetic sequencing to prove it.
“It’s fortuitous,” said Trevor Bedford, a biologist and genetics expert at Fred Hutchinson Cancer Research Center. “If you need to do sequencing to identify the variant you’re always going to be lagged a bit and it’s going to be more expensive. If you just rely on this S-dropout as identification then it’s easier.”
He said other variants also have sparked this quirk in PCR test results, but not the delta variant. With delta so dominant in the U.S. right now, an S-dropout result will get noticed, Bedford said. (Bedford receives funding from the Howard Hughes Medical Institute, which also supports The Associated Press Health and Science Department.)
Dr. Anthony Fauci, the nation’s top infectious disease expert, said it is “inevitable” that omicron will make its way into the United States.
Many experts said it’s probably already here and will be picked up by the surveillance system soon. But the question is, then what?
University of Wisconsin AIDS researcher David O’Connor noted: “We don’t have the sorts of interstate travel restrictions that would make it possible to contain the virus in any one place.”
Instead, genomic surveillance will tell officials if omicron is spreading unusually fast somewhere and whether more resources should be sent to those places, he said.
When omicron does surface, public health authorities will have to consider other variables in their triage efforts, such as the level of infection already present in that community and the vaccination rate. Serious outbreaks in highly vaccinated areas would be particularly concerning.
Still, the University of Minnesota’s Beckman sees little upside in vastly ramping up sequencing.
“You don’t need to sequence more than a few percent of positive cases to get a feel for how quickly it’s growing,” he said.
Unlike in some other countries, U.S. government officials haven’t exercised the authority to force people to quarantine if they test positive for worrisome variants. Given that, sequencing is mainly a surveillance tool for tracking mutations’ spread.
“I think it’s important to track variants, but I don’t think it’s practical to think that we’re going to be able to sequence quickly and broadly enough to stop a variant in its tracks,” Beckman said.
___
AP writers Lauran Neergaard, Matthew Perrone and Ricardo Alonso-Zaldivar contributed.
___
The Associated Press Health and Science Department receives support from the Howard Hughes Medical Institute’s Department of Science Education. The AP is solely responsible for all content.
Copyright 2021 The Associated Press. All rights reserved.
New York City mayor Bill de Blasio Monday “strongly recommended” every New Yorker, including fully-vaccinated people and those who have had the virus, should wear masks in all indoor public places due to the potential for the Omicron variant of COVID-19 to arrive. In a press conference yesterday, Governor Kathy Hochul said the situation is being closely monitored, and she fully expects it to arrive here…
Dr. Kirsten St. George is the Director of Virology at the New York Wadsworth Lab, and she says continuous monitoring of positive COVID specimens has not yet found any evidence of the new strain being in the country or the state…
The governor also says she’s concerned about the number of COVID hospitalizations trending up while the number of available hospital beds is going down.

Britain’s approach to coronavirus-related restrictions has been looser than other European countries, but the Omicron variant has spurred swift action on mitigation measures.
LONDON — At almost every step of the pandemic, Britain has been a coronavirus renegade. It locked down later than its European neighbors in March 2020, rolled out vaccines faster than almost any major country earlier this year, and threw off virtually all restrictions last summer in an audacious bid to return life to normal.
But with worries about a new variant, Omicron, flaring across the world, Britain has edged back in line with its neighbors in rushing to protect itself. Prime Minister Boris Johnson swiftly banned travel from 10 African countries, made face masks compulsory in shops and on public transportation, and on Tuesday greatly accelerated the deployment of vaccine booster shots, hoping to inject every adult by the end of January.
Britain’s approach is still significantly looser than countries like Austria, which are back in national lockdowns. People can gather in pubs without masks, for example, and officials keep promising weary Britons a normal Christmas. But Mr. Johnson said the government was prepared to stiffen its laissez-faire approach, at least for the moment, to stave off another wave of infection.
“We’re going to be throwing everything at it,” Mr. Johnson said at a Downing Street news conference. “We’re taking some proportionate precautionary measures while our scientists crack the Omicron code.”
Public-health experts welcomed the moves as a recognition that there are limits to Britain’s distinctive strategy, which combines a robust vaccination program with an almost total lack of restrictions since July. It showed, they said, that going it alone does not make sense with a fast-moving variant.
“The U.K. has reacted pretty promptly and basically initiated their Plan B, which many people like myself think they should have initiated a couple of months ago, to put off the threat of the new variant,” said Tim Spector, a professor of genetic epidemiology at King’s College London. “They are bringing the booster forward and making it available to anyone, which I think gives the right message.”
Under the new plan, Britain will expand eligibility for a booster shot to anyone 18 and older; they had previously been restricted to people over 40. It will shorten the time between shots to three months from six months, drawing on 400 military personnel to help deliver the extra doses. And it will offer a second vaccine shot to children aged 12 to 18, rather than only to those 16 or older.
The government will require all visitors to take a Covid test by the end of their second day after arrival in the country and quarantine until they receive a negative result. But officials brushed aside a call by the authorities in Scotland and Wales to impose a mandatory eight-day quarantine on all people who enter the country.
Even without the new variant, Britain has been reporting cases at a rate of more than 40,000 a day. The government has tolerated that high number because 80 percent of adults are fully vaccinated, which has weakened the link between infections and hospital admissions. About 30 percent of adults have gotten booster shots.
While the new regulations on travel and face masks bring Britain closer to other European countries, Professor Spector, who leads the Zoe Covid Study, which tracks Covid-19 symptoms, noted that “by comparison with other countries, the restrictions are still pretty mild.”
He also pointed out that Britain was slow out of the gate last week after news of the variant first emerged. It allowed passengers from African nations who landed in Britain to disperse into the country without testing them.
The government has stopped short of ordering people to work from home or mandated vaccine passports or masks in restaurants in England. France requires vaccine passports for restaurants. Spain and Italy mandate the wearing of masks in schools. In England, the Department of Education only advised students 12 and older to wear masks in communal areas, beginning Monday.
Mr. Johnson declined to advise people to cancel Christmas festivals, Nativity plays, or other social gatherings — parting company with one of his top health advisers, Jenny Harries, who said earlier that people should consider cutting back on socializing during the holiday season to curb potential transmission.
“I’m still confident that this Christmas will be considerably better than last Christmas,” said Mr. Johnson, alluding to the coal in British stockings last year after the rampaging Alpha variant forced the government to impose a lockdown.
Much of Britain’s strategy still hinges on its faith in vaccines, one of the few bright spots in its otherwise erratic response to the pandemic. Britain’s rapid rollout buoyed the Johnson government and gave it both the political capital and epidemiological case for easing pandemic restrictions in July — a policy it has stuck with even as the weather has chilled and cases remained stubbornly high.
“Our strategy is to buy the time we need to assess this variant,” the health minister, Sajid Javid, said on Tuesday. There are now 13 confirmed cases of the Omicron variant in England and nine in Scotland, he said, adding that it was not clear whether the most recent cases were linked to travel from Africa or community transmission.
The Omicron variant. The latest Covid-19 variant was identified on Nov. 25 by scientists in South Africa, though Dutch officials said two cases were detected in the Netherlands days earlier. Should you be concerned? Here are answers to common questions about this variant.
Travel restrictions and lockdowns. As more Omicron cases emerge globally, countries are responding in varied ways. Japan joined Israel and Morocco in barring all foreign travelers, and Australia delayed reopening its borders for two weeks. Here’s a list of where U.S. citizens can travel right now and what to know about travel restrictions.
A new type of treatment. A panel of advisers to the F.D.A is meeting to discuss an antiviral pill from Merck, the first in a new class of treatments that could work against a wide range of variants. The panel will vote on whether to recommend authorizing the drug for high-risk patients, which the F.D.A. could do within days.
Economic impact. Stocks fell sharply on Tuesday, driven by the likelihood that the Federal Reserve will hasten the removal of its supports for the economy just as Omicron has begun to spread. Meanwhile, analysts expect the markets to face weeks of uncertainty and increased volatility amid the new variant’s arrival.
On London’s busy streets, already twinkling with Christmas lights, some said the new rules seemed to be making a difference, after months in which mask-wearing habits had become rather desultory.
“Everyone’s wearing masks, and there’s a lot more police presence at stations,” said Joanne Cairns, 42, a marketing officer who arrived in London on Tuesday from the north of England.
But Matteo Grios, 32, said he found the patchwork of rules confusing. “Masks on public transport aren’t really going to stop the spread of the virus when you have big events happening at stadiums, or pubs where people get drunk,” he said.
Mr. Johnson’s reluctance to impose sweeping measures reflects pressure from his own Conservative Party. Experts say it is unlikely he would find robust support from restive lawmakers, some of whom flaunt their distaste for such measures by refusing to wear masks in Parliament.
While the House of Commons voted in favor of the mask mandate and travel restrictions on Tuesday, a handful of Conservative lawmakers warned against what they called the government’s authoritarian drift.
“Boris Johnson does face quite a lot of opposition on his backbench,” said Jill Rutter, a senior fellow at the Institute for Government, a London-based research group. She noted that he had alienated members with his handling of issues like a row over Conservative lawmakers who have lucrative second jobs.
Still, unlike last spring, when Mr. Johnson dragged his heels on imposing a travel ban on India after the emergence of the Delta variant, Britain acted quickly this time. Critics suggest he delayed putting India on a “red list” back then to avoid antagonizing New Delhi at a time when Britain was keen to strike a trade deal.
“The government has been stung by that criticism,” Dr. Rutter said.
Some experts chalk up Britain’s faster response to simple trial and error, after nearly two years of grappling with the ever-shifting challenges of the pandemic. On masks, for example, officials initially played down their efficacy, then urged people to wear them in confined spaces, before relaxing the guidance again in July.
“No country has found a good way of living with this virus,” said Devi Sridhar, head of the global public health program at the University of Edinburgh. “Going it alone with mixed strategies and restrictions has not worked out well.”
Saskia Solomon contributed reporting.
Enlarge / A baby with measles. CDC The Centers for Disease Control and Prevention is putting clinicians on alert about the growing r...
